Tick-borne encephalitis (TBE)
What is TBE?
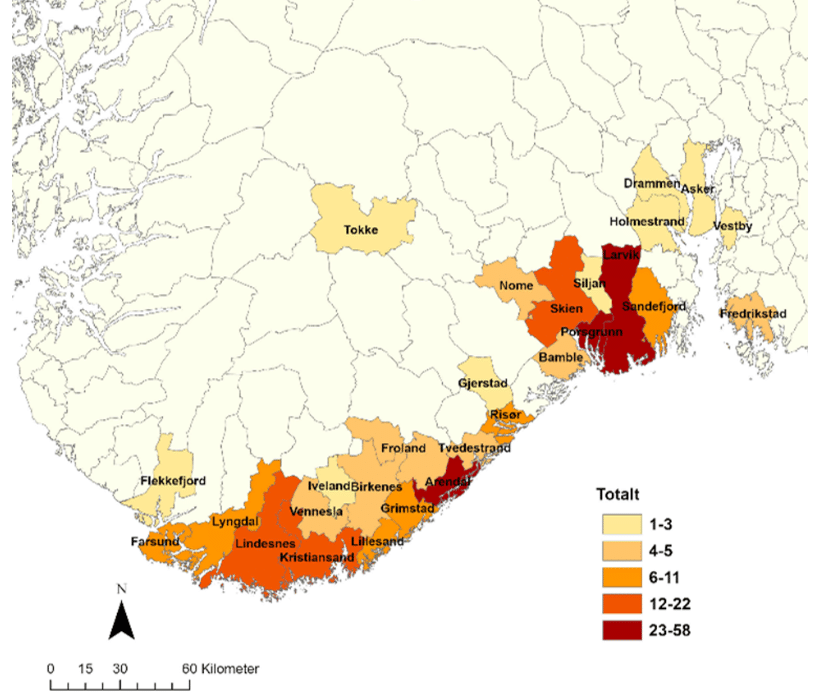
Tick-borne encephalitis (TBE) is caused by the TBE virus, a flavivirus. Subtypes include European, Siberian, and Far Eastern. In Norway, only the European subtype is present, transmitted by the sheep tick. The Siberian and Far Eastern subtype is mainly found in Eastern Europe to China and Japan. In rare cases abroad, consumption of unpasteurized milk or cheese from cows, goats and sheep can lead to infection. Symptoms vary greatly, from none to severe illness. Unlike borreliosis, where risk decreases if a tick is removed within 24 hours, TBE transmission can occur shortly after a bite. TBE incidence in Norwegian ticks is generally low but increasing. Less than 1% of ticks carry the virus on average, but local «hot spots» exist. In 2023, around 100 people in Norway were diagnosed with TBE, with a majority requiring hospitalization. To date, human TBE cases have only been reported in the following counties: Agder, Telemark, Vestfold, Akershus and Østfold (see figure below). Coastal areas in these counties are the risk areas for TBE in Norway.
Symptoms of TBE
The incubation period for TBE ranges from 2 to 28 days. While some individuals may experience no symptoms (asymptomatic infection) or only mild symptoms, others become very ill. A biphasic course of the disease is common, but not universal. The initial phase typically lasts about a week and resembles a «summer flu,» with symptoms such as moderate fever, headaches, muscle aches, and nausea/diarrhea. Some individuals may recover completely after this phase without realizing they were infected with the TBE virus, unless tested for TBE. However, others may experience a relapse with more severe symptoms (phase 2), including high fever, severe headache, lethargy, confusion, vomiting/diarrhea, neck stiffness, muscle aches, and paralysis. These symptoms indicate meningitis, encephalitis, and/or spinal cord inflammation. Adults, particularly the elderly, often experience a more severe illness compared to children. Hospitalization is common. The mortality rate for European TBE is less than 1%, while the Siberian and Far-Eastern types have higher mortality rates (up to 35%). In Norway, the first death due to TBE was recorded in 2022.
How is TBE diagnosed and treated?
The diagnosis of TBE is confirmed by detecting antibodies in blood and cerebrospinal fluid, along with inflammatory cells in the cerebrospinal fluid. In the early phase after infection, antibodies may not always be present in the blood, but TBE virus DNA can be detected early on with a PCR test. Approximately a week after infection, TBE antibodies (IgM and IgG) are formed. At this point, the PCR test is no longer positive because the viremic phase (the period when the virus is present in large quantities in the blood and tissues) has ended.